- September 1, 2020
- Posted by: Dr. Andi Fletcher
- Category: Blog

Making a Difference in the Health of California’s Underserved Children
Among the millions of children and young people in our communities, poor nutrition and sedentary lifestyles cause serious health issues and contribute to poor academic performance. Many of these children experience social and psychological problems and frequently miss school, and one in seven is too hungry to learn. Equally alarming is the likelihood that one in every three is likely to develop type 2 diabetes and other serious illnesses in his or her lifetime, with the number increasing to one in two for children of color.
If this pattern continues into adulthood, as it usually does, it will lead to an unprecedented rate of premature death and disability, diminished workplace productivity and staggering financial repercussions for families, insurers, healthcare providers and our society. We can, and must, reverse this trend. The good news is that children who develop healthy eating habits and are physically active at an early age are much more likely to maintain healthy lifestyles over their lifetimes. There is compelling evidence that publicly funded afterschool programs are uniquely well-positioned to do this.
In combination, more than a billion dollars in annual State After School Education and Safety Programs dollars, federal 21st Century Community Learning Centers appropriations and private and nonprofit investments already support over 4,000 school-based programs serving close to a million low-income children and young people every day. Students attend from the time school is out until 6:00pm at no cost to their families, an estimated 86 percent of whom are either covered by or eligible for MediCal insurance.
WHAT WORKS?
In 2004, the Center for Collaborative Solutions launched the Healthy Behaviors Initiative to test the effectiveness of using this platform to reach and improve the health of these youngsters. With multi-year funding from the Network for a Healthy California (a division of the California Department of Public Health), the David and Lucile Packard Foundation, The California Endowment, Kaiser Permanente and others, outcome-based practices were vetted by experts, embedded in multi-site programs serving over 100,000 elementary school students and field-tested in urban and rural communities across the state.
Based on the results, and the proven replicability of this approach in diverse organizational and geographic environments, Changing Lives, Saving Lives: A Step-by-Step Guide to Developing Exemplary Practices in Nutrition, Physical Activity and Food Security in Afterschool Programs was published in 2010. This was followed by case studies, professional journal publications, conference presentations and a second, updated edition of the Guide in 2015. To date:
- Healthy Behaviors Learning Centers, or world-class learning labs, have been certified and now train, coach and mentor other programs in throughout California.
- The California Department of Education’s Expanded Learning Division has made the promotion of healthy behaviors a priority for school districts and nonprofit organizations receiving State funding.
- 138 sites have been recognized by the Department of Education and the State Legislature as Distinguished After School Health Programs,
- And, most importantly, more than two million children and their families have benefitted.
WHAT’S CHANGING?
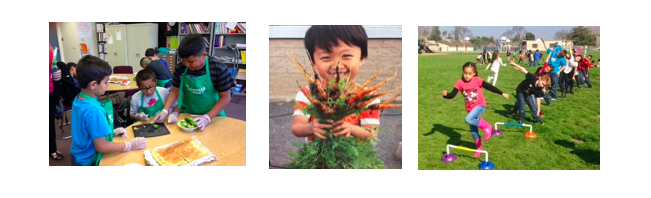
Children are becoming physically fit and improving their eating habits. According to independent evaluations, 87% of participating students are moderately to vigorously active at least 60 minutes a day. Many who previously failed State mandated Fitnessgram tests are passing, especially in the areas of endurance, strength and flexibility. An increasing number of those who were overweight or obese are reaching their desired weight, and 93% report that they enjoy exercising and understand why it is important.
Through hands-on experiences, children are becoming familiar with the basics of good nutrition, learning how to shop on a limited budget and preparing healthy snacks in their cooking classes and at home. Fifty-nine percent state that they are regularly choosing healthy foods over less healthy options, drinking more water and consuming fewer sodas. And, because programs include the USDA-funded Supper Program, all students have a healthy afternoon meal – one that for all too many may be their last until the school breakfast the next morning.
Staff and families are changing their behaviors. Staff members, who often live in the neighborhoods where their sites are located, and experience many of the same challenges as their students, are improving their own health and encouraging youngsters and their families to follow their lead. Literally tens of thousands of families are now taking greater advantage of community resources, participating in local health fairs, enrolling in the SNAP and WIC Programs and attending nutrition education classes. And over one-third of parents participating in focus groups reported that they are preparing healthier meals, eating more fresh fruits and vegetables and exercising more often.
Community partnerships are growing. Programs are working with community health centers, hospitals and local collaboratives to increase access to much-needed services for children and their families. Food banks, farmers markets, local growers and local businesses are making fresh produce more readily available and affordable. And, county offices of education, school districts and schools are focusing more on surrounding children with health-enhancing messages, adding salad bars to school lunch menus and planting gardens.
WHAT’S NEXT?
We are excited about the progress so far. And we know there is much more to be done. At the top of our list is making access to basic medical, dental, vision and other services more easily available. We believe that providing these during program hours can be a gateway to routine check-ups and care (for example, dental X-rays, cleanings and education and vision and hearing testing) and a way to identify increasingly common health issues such as early-onset Type 2 Diabetes.
Meeting children where they are eliminates transportation barriers and the need for parents to take time off from work – both of which are often serious challenges to preventative care for their children. It reduces cultural and language challenges and helps schools offset the impact of declining on-site health resources. It contributes to the ability of insurance providers to meet their MediCal service goals. And, most importantly, it has the potential to significantly increase the number of children who receive the healthcare services they desperately need.
